The Common Vein Copyright 2012
Introduction
Arteries are composed of three layers:
Tunica intima
Tunica media
Tunica adeventitia
Tunica intima:
The tunica intima is the innermost layer of an artery. It is a transparent structure that is highly elastic. The tunica intima is made out of a layer of endothelial cells. There is a subendothelial layer that has delicate connective tissues. These connective tissues consist of a single stratum of stellate cells, and the tissue is only largely developed in vessels. There is an elastic layer which consists of a membrane containing a network of elastic fibers. This membrane forms the main thickness of the inner coat. It can be separated into several layers, showing the network of elastic fibers.
Tunica media:
The tunica media is the middle layer of an artery. It lies between the tunica intima on the inside and the tunica adeventitia on the outside. It is made up of smooth muscle cells and elastic tissue. The tunica media is distinguished by its color and by the arrangement of its fibers. In smaller arteries, it consists of plain muscle fibers. In larger arteries, elastic fibers unite to form a lamella which alternate with the layers of muscular fibers. These fibers are connected with the membrane of the tunica intima. In the largest arteries, there are a few bundles of white connective tissue that are wrapped around the tunica media.
Tunica adventitia:
The tunica adventitia is the outer layer of an artery, it surrounds the tunica media. It is mainly composed of collagen and is supported by external elastic lamina. The collagen that the tunica adventitia has serves as an anchor to the blood vessel to nearby organs, giving it stability.
In the Heart
Histology
Ganesh Athappan MD Ashley Davidoff MD
Introduction
The layers of the heart conform to the basic pattern seen in the histology of other tubular structure except that the muscle layer dominates.
Tubular structures in the body have a basic structural makeup of an inner layer lined with an epithelial layer abutting the lumen, a middle functional layer and an outer protective layer or skin. In the heart the inner layer is called the endocardium, middle muscular layer is called the myocardium, and the outer layer is called the pericardium.

The Three Layers of the Wall of the Heart |
|
The histological section shows the inner layer called the endocardium (endo) which lines the inner portion of the cavity and the myocardium (myo) is the middle layer which in this case is relatively thin since it is from the atrium, and then the outer pericardium (peri). Courtesy Ashley Davidoff MD copyright 2009 06620c02.8s |
The layers are complex in their makeup. The endocardium consists of an endothelial layer which rests on a subendothelial layer and basement membrane. Between the endocardium and myocardium there is a subendocardial layer. The myocardial layer is complex in the manner in which the myocardial cells are oriented and organized. The pericardial layer consists of two basic layers between which is the pericardial space, and each of which is made of unique tissue.
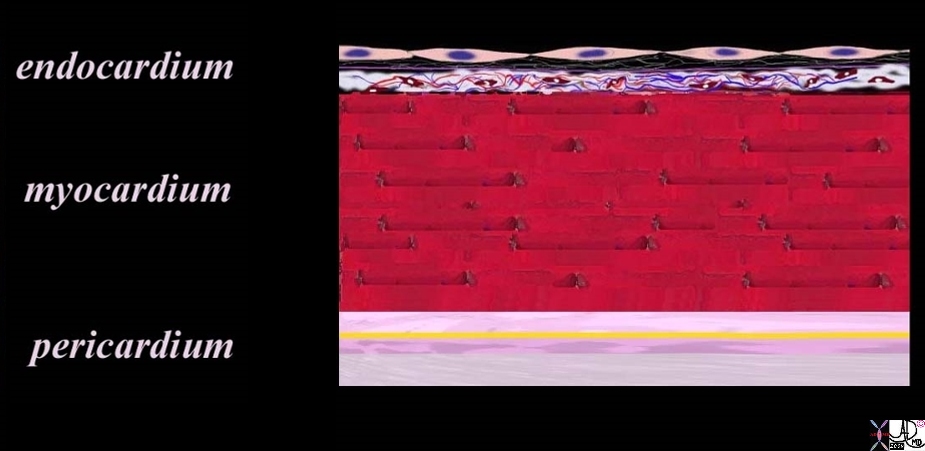
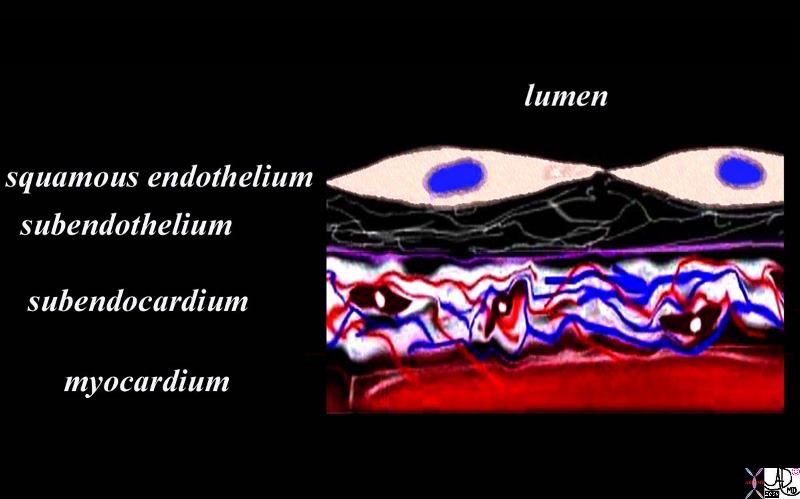
Diagram of the Parts and Subparts of the Wall of the Heart |
|
The diagram shows the three basic layers of the heart; the endocardium myocardium, and pericardium The endocardium consists of an endothelial layer made of a single layer of squamous cells abutting the cardiac cavity. Below this layer there is a fine network of collagen fibers and a basement membrane. The fine collagen layer and basement membrane together are called the subendothelial layer. The endothelium is anchored by the basement membrane. Below the basement membrane is the subendocardium which consists of dense collagen elastic tissue, capillary network, arterioles, venules, smooth muscle cells and elastic tissue. The maroon tissue below this layer is the myocardium. External to the myocardium is the pericardium which consists of an inner visceral pericardium, (light pink) the pericardial space (yellow), and an outer parietal pericardial layer. The outer parietal pericardium consists of an inner seroelastic layer (dark pink) and outer fibrous layer (gray) Courtesy Ashley Davidoff MD 86815b22.9s copyright 2009 |
Principles
Endocardium:
The endocardium consists of a single layer of squamous endothelial cells that rests on a layer of fine collagen fibers and a basement membrane.
The squamous endothelial cells are shaped like the scales of a fish and have oval or round nuclei. The squamous lining of the entire heart is continuous with the endothelial cells lining all the vessels in the body forming one large sheet of tissue spread throughout the entire cardiovascular system. Perhaps one can think of it as a tubular table cloth that extends from the toes to the head –one long, extensive, and remarkable sheet of tissue.
The endothelium rests on a continuous layer of fine collagen fibers, which is itself anchored by a basement membrane. These two structures (fine collagen layer and basement membrane) form the subendothelium. Beneath the subendothelium is a thicker layer of dense connective tissue forming the subendocardium. It is composed of collagen fibers , elastic fibers , smooth muscle cells , small blood vessels, and in the ventricles may contain specialized cardiac muscle cells of the conduction system . The connective tissue in this region binds the endocardium to the myocardium.
The endocardium is variable in thickness, being thickest in the atria (left > right) and thinnest in the ventricles particularly the left ventricle. Localized areas of endocardial thickening (jet lesions) are common, particularly in the atria, as a result from turbulent blood flow within the chamber.
|
Endocardium Subendocardium and Myocardium
|
|
The diagram shows the endothelial layer consisting of a single layer of squamous cells abutting the cardiac lumen. Below this layer there is a fine network of collagen fibers and a basement membrane (purple) . The fine collagen layer and basement membrane together are called the subendothelial layer. The endothelium is anchored by the basement membrane. Below the basement membrane is the subendocardium which consists of dense collagen elastic tissue, capillary network, arterioles, venules, smooth muscle cells and elastic tissue. The red tissue below this layer is the myocardium. The subendocardium is the equivalent of the submucosa that brings the lifelines of vessels and nerves to the cellular level. Courtesy Ashley Davidoff MD Davidoff art copyright 2009 86815b14.8s |
Macroscopically the endothelial surface is shiny, smooth, and moist.

The Glistening Endothelium |
|
The post mortem specimen reveals the opened the left atrium and a view of the anterior leaflet (al) and the posterior leaflet (pl) of the mitral valve. The patent foramen ovale is shown on the septal side of the left atrium. The glistening surface of the endothelium is seen throughout the LA, extending seamlessly onto the mitral valve. It is seen in cross section (white arrow) as part of the white endocardium, together with a thin myocardial layer (maroon arrow) and pericardial layer (pink arrow). Courtesy Ashley Davidoff MD copyright 2009 all rights reserved 01791c01.8s |

Shining Glistening Endothelium of the Left Ventricle |
|
The left ventricle that has been opened along the ventricular septum shows the septal wall to your left and the free wall with the papillary muscles to your right. Note the glistening endothelium which has a whitish sheen. The myocardium lies directly under the endocardium.. Note also the two sets of papillary muscles, and the fibrous continuity of the mitral valve with the aortic valve. A VSD is noted on the superior aspect of the septum. Courtesy Ashley Davidoff all rights reserved copyright 2009 08345b.8 |
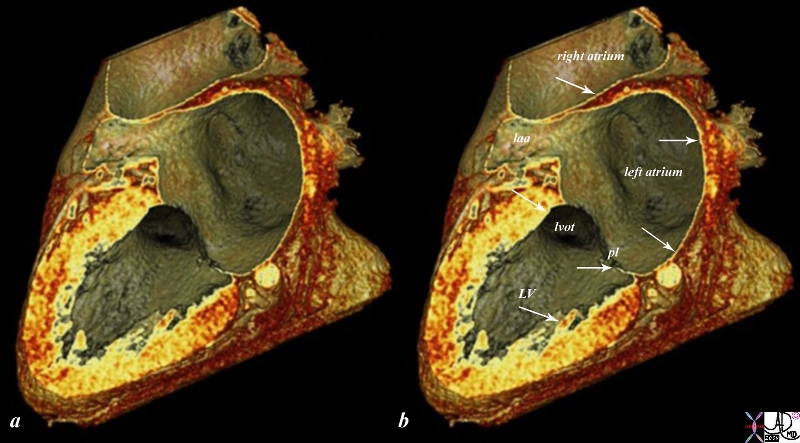
CTscan of the Endocardium |
|
The reconstructed CTscan shows the thin endocardium (white arrows) throughout the heart – which is in fact one continuous sheet of tissue connected across the whole circulatory system. The thin white layer is seen in the left atrium, left atrial appendage (laa) over the posterior leaflet of the mitral valve (pl), in the left ventricle (LV) and in the right atrium. The surface of the left ventricle, left ventricular outflow tract (lvot) and right atrium are also lined by the endothelium. Courtesy Ashley Davidoff MD copyright 2009 all rights reserved 47824c02.8s |
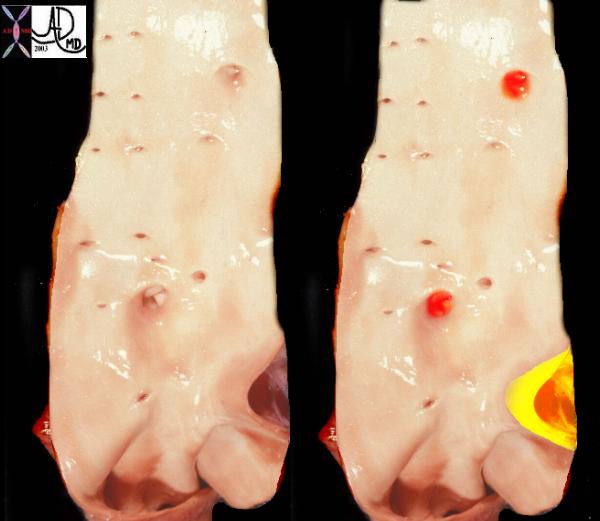
There are certain diseases that cause thickening of the endocardium usually caused by subendocardial ischemia. Endocardial fibroelastosis (EFE) which is seen in the endocardium of the left ventricle in hypoplastic left heart syndrome is shown below. The entity is thought to result from ischemic changes induced by the suprasystemic pressures in the left ventricle caused by severe left ventricular outflow obstruction and resulting in subendocardial ischemia and secondary fibrosis.
|
Endocardial Fibroelastosis |
|
The grosspathology specimen is a case of hypoplastic left heart with aortic stenosis and mitral stenosis, revealing a thickened endocardium with left ventricular hypertrophy, deformed and thickened mitral valve and papillary muscles. The thickened endocardium is caused by the high pressures generated in the LV causing subendocardial ischemia and a resulting in a condition called endocardial fibroelastosis. (EFE) Copyright 2009 Courtesy Ashley Davidoff 08058.8s |
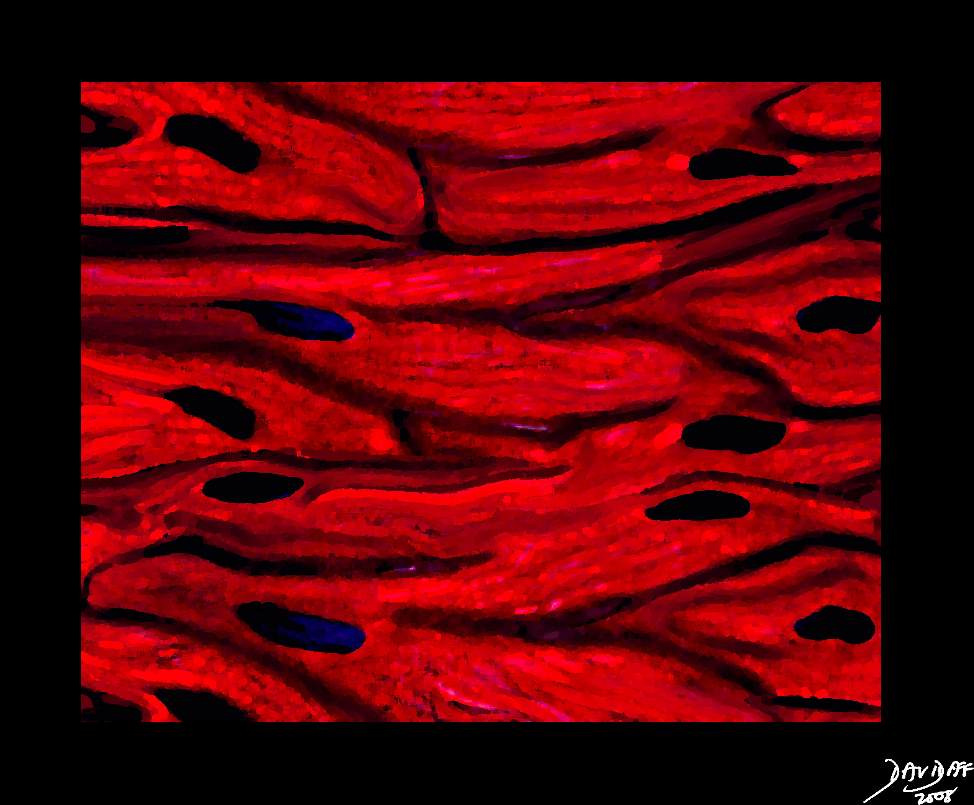
Myocardium:
The myocardium is made up of layers of cardiac myocytes (75% of the total volume of the myocardium), attached to each other by connective tissue fibers, and arranged in spiral bundles. The myocardium is the contractile layer of the heart and hence the major function of myocardial muscle cells is to execute the cardiac contraction-relaxation cycle. The cell is striated, with a single nucleus, with dark staining intercalated discs. It is thickest in the left ventricle and thinnest in the atria. The overall architecture is one of muscles arranged in spiral and circular bundles.
|
32907b03.61k.8s |
|
A drawing of the histology of the myocytes of the heart showing how they are connected and related as a continuum enabling a coordinated contraction pattern. Note that the cell membranes are interrupted allowing the cells to freely communicate with each other. This arrangement is called a syncitium – an open door approach of the cells to allow efficient communication and connection. Courtesy Ashley Davidoff MD. 32907b03.61k.8s copyright 2009 |
|
Low Power View of the Myocardium |
|
The myocytes tend to be long, thin, and slightly rectangular. The nuclii are round and blue. Connective tissue between the muscle cells is seen as pale pink collagenous material in which parts of blood vessels can be seen. 03885b01 Courtesy Ashley Davidoff copyright 2009 |
Ventricular Myocytes
The muscles of the ventricles are arranged as
(1) external longitudinal layer
(2) middle circular and
(3) inner longitudinal layer.
Isolated bundles of cardiac muscles project into the lumen of the ventricle forming the trabeculae carnea.
The overall architecture of the myocardium of the left ventricle is in the form of a figure of 8 with one side attached to the subendocardium and then a gradual helical twist almost to 180 degrees as it extends to the subepicardial surface.
A myofiber or myocyte is the basic structural and functional unit of the myocardium. The cells are held together by surrounding collagenous connective tissue with strands of collagen also connecting the myofibers to each other. Within the myofiber there are myofibrils.
Light Microscopic Details of the Cardiac Myocyte:
The myocyte is composed of myofibrils, mitochondria, T systems, sarcoplasmic reticula, embedded within the cytoplasm.
Under the light microscope, the atrial and ventricular myocytes have cross striations and are branched and often contain two nuclii. Each myocyte is bound by a complex cell membrane, the sarcolemma and is filled with rod-like bundles of myofibrils . The latter are the contractile elements.
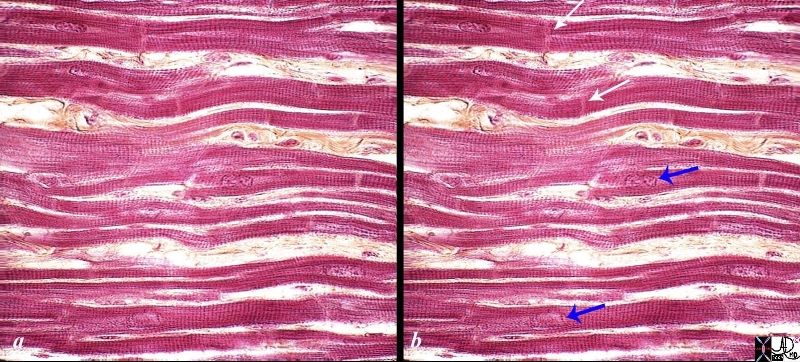
High Power of the Myocardium |
|
The histological slide shows normal myocardium with the white arrows pointing to the borders between two cells at the intercalated discs. The blue arrows point to the nuclii of the cells. The cross striations are very obvious, while the longitudinal striations are a little more difficult to visualize. Connective tissue can be seen between the cells (myocytes). 86816c02.8s Source unknown |
Characteristics of ventricular myocytes:
Size;
Length : 60-140 μm (red cell about 5 μm and liver cell about 20-30 μm)
Diameter: about 20 μm
Volume : 15,000-45,000cubic μm
Shape:
Long and narrow
Ventricular myocytes have branching bundles allowing the cells to connect both structurally and functionally as a syncitium. There is little interstitial collagen but abundant mitochondria and sarcomeres.
Character
Syncitial arrangement
Intercalated discs are prominent with end to end transmission.
T tubules are plentiful (invagination of the sarcolemma)
The sarcolemma of the myocyte invaginates the cytoplasm to form an extensive tubular network (the T tubules) that extends the extracellular space into the interior of the cell. The nucleus, which contains the cell’s genetic information, is often centrally located. Some myocytes have several nuclei. Interspersed between the myofibrils and immediately beneath the sarcolemma are many mitochondria, the main function of which is to generate the energy in the form of adenosine triphosphate (ATP) needed to maintain the heart’s contractile function and the associated ion gradients. The sarcoplasmic reticulum (SR) is a fine network spreading throughout the myocytes, demarcated by a lipid bilayer, which is similar to that of the sarcolemma. The calcium release channels (also called the ryanodine receptors) are found in the expanded parts of the SR that lie in very close and in apposition to the T tubules. These are called subsarcolemmal cisternae or the junctional SR. The second part of the SR, the longitudinal or network SR, consists of ramifying tubules and is involved with the uptake of calcium that initiates relaxation. Calcium is taken up into the SR, and is then stored at high concentration in a number of storage proteins, including calsequestrin, before being released again. The cell boundaries are seen as thin, typically dark-staining lines dividing adjacent cardiac muscle cells. They are called the intercalated discs.
The manner in which the myocytes are arranged for optimal performance is quite an ingenious trick of nature. With about 15% myocyte shortening the heart can eject between 55-65% of its load. In the mid body the cells are circumferentially arranged and are twisted one way under the subendocardium and twisted the opposite way below the epicardium. During systole this allows for shortening in both the axial plane and along the long axis as well as allowing for a wringing or twisting type action to the pattern of contraction. The base moves clockwise and the apex moves counterclockwise. This type of wringing action, (likened to the wringing action one performs to dry a wet towel) not only allows for efficient emptying but also is thought to have a vacuum effect as relaxation occurs.
Atrial Myocytes:
The muscles of the atria extend as an arc from the front to back and partly diagonally across the atria from one side to the other . Bundles of atrial tissue are separated by wide areas of collagen. Prominent bundles of atrial muscles form the pectinate muscles. Atrial myocytes are the basic structural and functional unit of the atrium. The characteristics of atrial myocytes are slightly different to the ventricular myocytes:
Size
In general the atrial myocyte is much shorter, thinner, and less voluminous than the ventricular myocyte. T tubules are rare whereas in ventricular muscle they are abundant.
Length : 20 μm
Diameter: 5-6 μm
Volume : approx 500 cubic μm
Shape:
Elliptical
Character
T tubules are rare
Intercalated discs with side to side and end to end transmission.
Some myocytes in the RA and fewer in the LA have neurosecretory granules for atrial natriuretic peptide.
Pericardium:
The pericardium consists of two basic layers. There is an inner layer called the visceral pericardium that is made of a layer of fibroelastic connective tissue blood vessels, lymphatics, nerve fibres, and a variable amount of adipose tissue that merges with the myocardium. The second layer called the parietal pericardium is more superficial layer, and is made up of a tougher fibroelastic layer called the fibrous pericardium and a more delicate mesothelial serous lining.
Visceral Pericardium
The epicardium (or visceral pericardium) forms the outer covering of the heart. (Cormack). Its free surface is composed of a single layer of flat to cuboidal mesothelial cells resting on a layer of connective tissue rich in elastic fibers. The subepicardial space adjacent to the myocardium contains blood vessels, nerves and abundance of fat cells.
Parietal pericardium
The parietal pericardium has two parts; an inner portion that has a serous lining and an outer fibrous component. The latter is made from collagen with a small amount of elastin. The collagen is organized in criss-cross pattern.
When the inner single cell thick cuboidal mesothelial surface of the linings of both the parietal and visceral pericardium are reviewed under the electron microscope they reveal microvilli and long cilia which secrete fluid and provide a low friction surface.
Below the mesothelial epithelia a layer of elastic fibrils supports the epithelium.
There is a rich network of lymphatics that provide the substrate for the pericardial fluid.
Fibrous Skeleton:
The fibrous skeleton of the heart , formed of connective tissue, separates the atria from the ventricles and includes the annuli fibrosi – (rings of dense connective tissue around the valves), trigona fibrosi ( masses of fibrous connective tissue connecting the annuli) and the septum membranicum (membranous spot at the top of the interventricular septum). It is composed of dense collagen fibers, scattered elastic fibers and occasional fat cells. (less regular than tendon, more regular than dermis). The cardiac skeleton serves as the place of origin and attachment of muscles of the atria and ventricles.
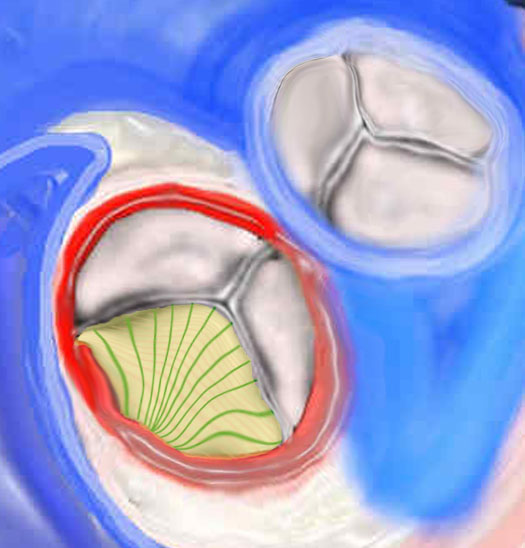
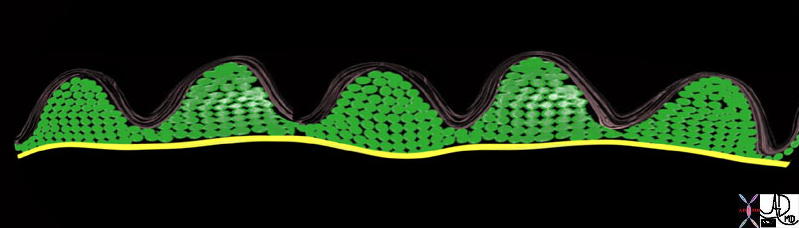
Valve Leaflets
Valve leaflets are composed of three layers (ventricularis, fibrosa and spongiosa) and two general cell types (1) endothelium – non thrombogenic external lining and valvular interstitial cells – heterogeneous cell population composed of fibroblast and smooth muscle cells. The cardiac valves are lined with endothelium and all have a similar three- layered architecture consisting predominantly of a dense collagenous core, the fibrosa layer, close to the outflow surface and continuous with the valvular supporting structures. Towards the ventricular/atrial cavity the ventricualis/atrialis layer is found and it is rich in elastin. Between these two layers is the centrally located core of loose connective tissue, the spongiosa layer. The collagen of the fibrosa layer is responsible for the mechanical strength of the valve, whereas the connective tissue of the spongiosa layer works as a shock-absorber. Normal leaflets and cusps have only scant blood vessels and are avascular structures.
|
Histological Makeup of the Aortic Valve |
|
There are 3 layers of collagen within the valve. The first image (top) shows the fibrosa layer on the aortic side of the valve. (pink) This layer consists of radially oriented fibers extending from commissure to commissure. It has corrugated form enabling it to stretch during systole. The second middle layer is called the spongiosa green and its fibers extend at right angles to the fibers of the fibrosa. On the ventricular side in the third image a cross section of the histological makeup of the aortic valve is shown with the upper layer being on the aortic side and the yellow layer of ventricularis is shown. The ventricularis is a sheet of tissue called. (yellow) 47682d07 47682d03 47682eb06.800 Copyright 2009 Courtesy Ashley Davidoff Davidoff art |
Histology of the Cardiac Conduction System :
The conduction system is made of myocardial fibers designed for rhythm rather than contraction. They include the nodal cells ( AV nodal , SA nodal) and the AV bundle along with its branches (Purkinje cells).
Nodal Cells: Nodal cells are smaller than ordinary cardiac myocytes, contain fewer and poorly organized myofibrils and no intercalated discs.
Purkinje cells: They are specialized myocytes found in the subendocardium of the ventricles. Purkinje cells are rich in glycogen and mitochondria and often have two more nuclei centrally placed.
Charactersitics of Purkinje cells:
Size :
length 150-200μm
diameter : 35– 40μm
Volume : 135,000-250,000 cubic μm
Shape :
Long and broad , lighter staining and with abundant sarcoplasm and scarce sarcomere
Character
T- Tubules are absent
Intercalated discs are very prominent with abundant gap junctions for fast end-to-end transmission.
In the Aorta
Histology
The Common Vein Copyright 2007
Ashley Davidoff Cristina Cesaro
The aortic wall, with its high elastic content supported by muscle and collagen, allows for transmission of a more or less steady blood pressure within the circulation by providing a tensile strength that can be adjusted to conform to the pumping strength of the heart muscle.
 Normal Smooth glistening Endothelial Surface of the Neonatal Aorta Normal Smooth glistening Endothelial Surface of the Neonatal Aorta
|
| This is a post mortem specimen of the aorta of a patient with pulmonary atresia and bronchial collaterals. Overlaid in red are the enlarged orifices of the origins of the bronchial arteries. In yellow is the entrance of the PDA (patent ductus arteriosus) to the aorta Note in addition the normal appearing shiny appearance of the neonatal intima. Courtesy Ashley Davidoff MD 32628c a79-8 |
The composition of the aortic walls attributes its elastic nature. The innermost layer of the artery is the tunic intima. This layer is coated by a single sheet of endothelial cells which line the lumen of the artery. The intima’s subendothelial layer consists of a complex network of cells which aid in the dilation and contraction of the walls. They include fibroblasts, macrophages and elastic fibers surrounded by in an extracellular matrix. These membrane-bound elastic fibers run in parallel directions, causing the striated appearance of the layer.
Directly below the intima lies the tunica media. Composed primarily of smooth muscle and elastic fibers, this is the layer primarily responsible for the aorta’s distensible strength. The elastic fibers are discretely packaged in circulatory lamellae separated by an intercellular medley of elastic fibers, collagen and undifferentiated cells. Such a radial arrangement of fibers characterizes this middle layer.
The last and outermost layer of the aorta is the tunica adventitia. Extending to the outer wall of the aorta, this layer serves not only as a protective covering for the aorta but also a supplier of oxygen to the distal layers of the wall. This function is achieved by the vasa vasorum—an extensive network of miniscule arterioles dispersed between the media and adventitia interface. It should be noted that these branches vary along the sections of the aorta. They are most dense in the thoracic region and nearly absent in the abdominal region. Without the vasa vasorum, only the proximal aortic layers would receive substantial oxygen from the lumen. In comparison with the tunica media, the tunica adventitia contains a smaller amount of smooth muscles cells. It is primarily made up of collagen-dispersed connective tissue, fibroblasts and a network of nerves relaying mostly adrenergic responses. These fibers protect the aorta from overstretching and comprise the aorta’s protective outer shell.
 Elastic Artery Elastic Artery |
| 47678b04.800 artery aorta histology character normal endothelium media adventitia tunica elastica tunica muscularis. |
 Elastic Aorta Elastic Aorta |
| histologic section of the wall of the aorta shows the thin intima, the thick elastic media characterised by the white wavy bands, and the media which consists of strong collagenous fibres.
|
 Elastic Aorta Elastic Aorta |
| 47678.800 artery aorta histology character normal endothelium media adventitia tunica elastica tunica muscularis Davidoff art Davidof MD |
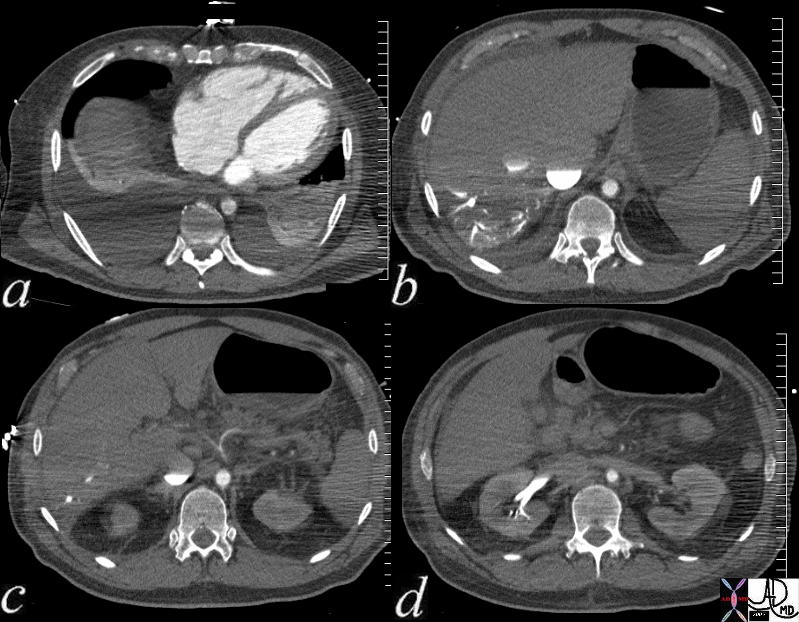 Shock and the Small Aorta Ability of the Smooth Muscle Shock and the Small Aorta Ability of the Smooth Muscle |
| This patient presents with cardiogenic shock In image a, the right ventricle and right atrium are enlarged and thereare bilateral pleura; effusions. Image b shows stasis of contrast into the IVC and the column is relatively stattic due to peripheral constriction and slow return. There is reflux into the hepatic veins due to tricuspid regurgitation and the reflux extnds all the way to the periphery indicating poor forward flow in the hepatic circulaltion again due to operipheral constriction. Note how small the aorta due to contraction of the muscular media in this life threatening situation.. In image c the celiac axis with branches hepatic artery and splenic artery show severe vasoconstriction. In d the reflux of contrast from tricuspid regurgitaion (TR)extends deep into the renal parenchyma for the reasons outlined above. The patient subsequently developed shocked liver.
73796c01 Courtesy Ashley Davidoff MD |